Introduction
Even after effective treatment of the Borrelia burgdorferi infection, Lyme Disease can have long-lasting consequences.
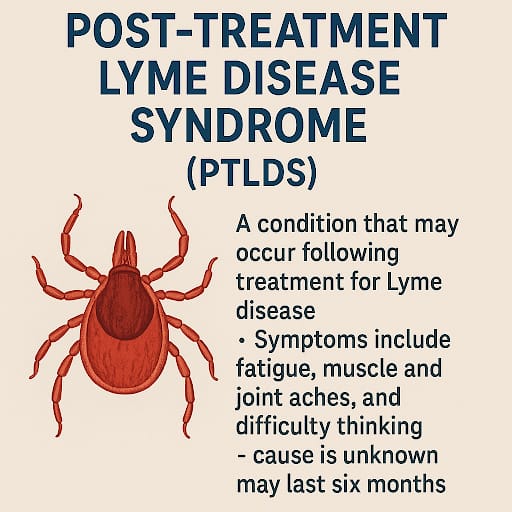
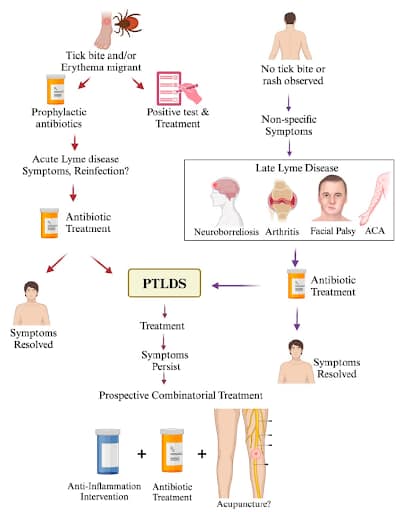
This condition is termed as Post-Treatment Lyme Disease Syndrome (PTLDS). PTLDS can involve uncontrolled fatigue, pain, and problems with cognitive functions after effective treatment even if there is no trace of bacterial presence.
Such discussion would help one understand both the management of PTLDS as well as differentiate chronic Lyme disease complexities. To enhance your knowledge in PTLDS, the most important parts of PTLDS are discussed below along with their answers.
What is Post-Treatment Lyme Disease Syndrome (PTLDS)?
- Post Treatment Lyme Disease Syndrome (PTLDS), can be described as a condition in which the symptoms of Lyme disease persists even after the patient is treated with antibiotics.
- Because completing the dosage of the prescribed antibiotics does not lead to healing, and if the Lyme Symptoms still persist, it is referred to as the Post Treatment Lyme Disease Syndrome.
- Symptoms like cognitive difficulties, joint pain, as well as profound fatigue, which are termed noticeable symptoms, appear within six months and last longer than that.
- The reasons underlying the development of this syndrome are unclear but, it could possibly be the result of the immune reaction or remains of the bacteria or damage to the tissues of the body during infection.
What are common PTLDS symptoms?
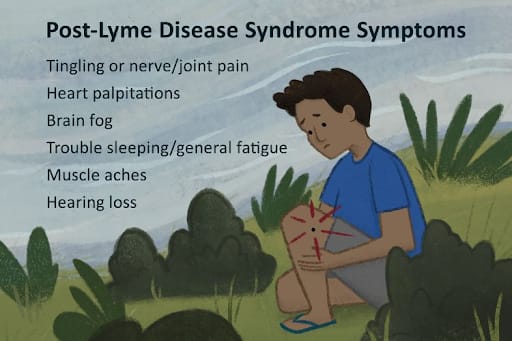
- The common symptoms presented include fatigue, pain in muscles or in the joints, issues with memory, and difficulty concentrating. These symptoms are difficult to manage because of their great impact on quality of life.
- Even after the treatment of Lyme disease, PTLDS patients show a clinical observation of symptoms that need to be diagnosed accurately to find a lasting therapy that helps the patient in every way.
- While they still sound mildly troublesome, when shown at a higher intensity, they tend to get in the way of patients being able to complete everyday activities.
- It is also common for these patients to face additional issues ranging from mood swings, sleeping disorders, and unexpected light or sound sensitivity.
How is Post-Treatment Lyme Disease Syndrome (PTLDS) diagnosed?
- PTLDS isn’t diagnosed in a single test available. However, a mix of a person’s medical history, treatment of Lyme disease, and observing any persistent symptoms could ensure a more straightforward diagnosis.
- An important thing to keep in mind for PTLDS patients is being troubled by chronic fatigue or having aches in multiple body spots for periods exceeding weeks for a maximum of six months.
- Always remember that long term solutions to combat PTLDS symptoms require eliminating other potential causes of the exhibited symptoms.
What are the long-term effects of Lyme disease?
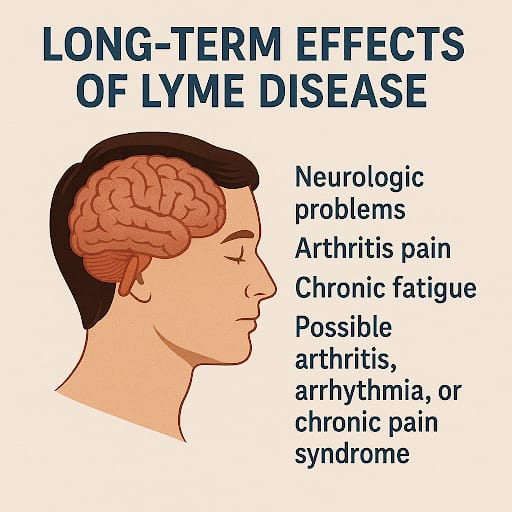
- Long-term effects of Lyme disease can result in neurologic problems, arthritis pain, or chronic fatigue that can last for months or even years if untreated or mismanaged.
- As expressed earlier, complications of Lyme disease’s long-term effects can frustrate joint mobility, create memory issues or peripheral neuropathy pain.
- Possibility of Lyme disease may also increase due to probable arthritis, arrhythmia, and chronic pain syndrome. These observations substantiate the significant need to treat patients at the early phases of the disease to stop its progress and further complications.
- In order for a patient to return to being functional, there needs to be sufficient therapy and management of the patient.
What treatments are available for PTLDS?
- PTLDS treatments target the unresolved signs and symptoms with medications, physical exercises, cognitive rehabilitation, and/or psychotherapy. The use of antibiotics is not suggested for persisting symptoms.
- The intent behind treating PTLDS is to manage symptoms, as prolonged use of antibiotics yields no positive outcomes. Assisting with pain, as well as muscle relaxation therapy, helps with easing the musculoskeletal symptoms.
- Neurological problems are addressed by counseling and cognitive rehabilitation therapy. Incorporating mindfulness practices, acupuncture, and dietary changes can improve health. There has to be a baseline upon which to build and follow a care plan for each and every patient based on the exact symptoms presented and needs identified.
Conclusion
- Taking care of PTLDS is one of the critical considerations in improving outcome measures for patients.
- Addressing lifestyle and waiting at the right moment to intervene or provide diagnostic support can significantly reduce the effects of Lyme disease.
- Having PTLDS and dealing with its symptoms is difficult, but allows individuals to return to living a better life.
References
- Dersch R, Sommer H, Rauer S, Meerpohl JJ. Prevalence and spectrum of residual symptoms in Lyme neuroborreliosis after pharmacological treatment: a systematic review. J Neurol. 2016; 263(1): 17-24. PubMed
- Wormser GP, Weitzner E, McKenna D, et al. Long-term assessment of health-related quality of life in patients with culture-confirmed early Lyme disease. Clin Infect Dis. 2015; 61(2): 244-247. PubMed.
- asq ES, Bujak DI, Weiss M, Peterson MG, Weinstein A. Lyme disease: an infectious and postinfectious syndrome. J Rheumatol. 1994; 21(3): 454-461. PubMed.
- Wormser GP, Dattwyler RJ, Shapiro ED, et al. The clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006; 43(9): 1089-1134. PubMed.
- Marques A. Persistent symptoms after treatment of Lyme disease. Infect Dis Clin N Am. 2022; 36(3): 621-638. PubMed. Google Scholar PubMed


