Lyme disease is a bacterial infection and can result in clinical symptoms, such as skin rashes, fever, musculoskeletal pain, etc. Can Lyme disease cause jaw pain? In some patients, Lyme disease affects the temporomandibular joint (TMJ) that can lead to stiffness and discomfort.
This can create confusion among dentists and doctors. If the real culprit is not detected, there can be misdiagnosis and unnecessary treatments. In this blog, we will explore how Lyme disease and TMJ pain are related.
What are the causes of temporomandibular joint dysfunction?
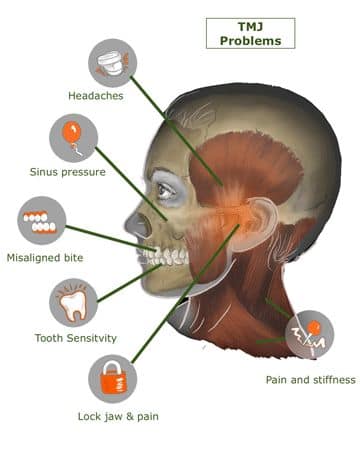
The temporomandibular joint connects the lower jaw to the skull. These joints help the mandible to move upward, downward, forward, and backward. Several actions, like chewing, swallowing, talking, etc, take place with the help of proper alignment between joints and mandibles. Temporomandibular joints disorders affect the nerves, jaw muscles, and temporomandibular joint.
TMD can be classified into three types:
- Degenerative joint disease: This type comprises osteoarthritis or rheumatoid arthritis.
- Myofascial pain: This type can result in pain/discomfort in the connective tissue that covers the muscles.
- Internal derangement of the joint: In this type, there will be dislocation of the jaw or disk displacement.
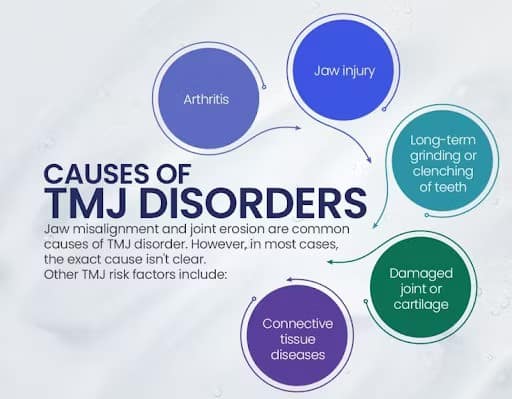
Causes:
- Dislocated jaw
- Bruxism
- Arthritis in the jaw joint
- Increased stress levels
- Trauma to the head or neck region
Symptoms:
- Clicking of the jaw
- Clenching of teeth
- Trouble in opening and closing the mouth
- Headache
- Tingling sensation
- Restricted movement
How are Lyme disease and TMJ related?
Lyme disease can have an impact on the musculoskeletal and nervous systems. The infection is caused by the bacterium, “Borrelia burgdorferi”, which can cause inflammation in the surrounding tissues and joints. As a result of the inflammatory response, Lyme disease can result in arthritis. Due to the inflammation, there will be pain and stiffness around the jaw.
There can be muscle spasms that affect the TMJ muscles (temporalis and masseter). This can often result in clenching of the jaws and grinding of teeth. Lyme disease can affect the nerves that control the movement of the jaws.
When there is inflammation/irritation of the nerve, TMJ symptoms can worsen. Mostly, the clinical symptoms will be misdiagnosed as a dental or ENT issue. Hence, the actual cause remains undetected. If there are systemic symptoms (fatigue, fever, etc.), Lyme disease must be suspected.
Case study
A 25-year old female patient had clinical symptoms of TMJ disorder. Initially, removable/fixed orthodontic appliances were provided. She was also provided a bruxism splint due to the presence of facets on teeth. After three months, she woke up with an intense pain in the right TMJ. When she repositioned her lower jaw, a cracking sound was heard. Later, she suffered from constant pain and restricted mouth opening.
A dental splint, along with the mouth opening exercises and physiotherapy, was suggested as the treatment modality. Over time, clinical symptoms worsened. NSAIDs were prescribed to reduce the pain. Unfortunately, the pain was not relieved and the patient also experienced an allergic reaction. Blood tests revealed the presence of the antibodies (IgG & IgM). The serological findings confirmed the presence of Lyme arthritis that affects the right TMJ.
Antibiotics (Cefuroxime) were administered intravenously for three weeks. A one-week course of antibiotic treatment improved the clinical symptoms. Diagnostic errors can be prevented by consulting a specialist and initiating proper treatment.
What are the available treatment strategies for managing TMJ pain related to Lyme disease?
Lyme disease can result in TMJ pain that requires a comprehensive approach to address the underlying symptoms. The primary treatment is the antibiotic therapy that helps in eliminating the bacteria. Early stages of Lyme disease can be managed with amoxicillin or doxycycline. In advanced cases, intravenous administration of antibiotics is necessary. Non steroidal anti-inflammatory drugs can be used to relieve the joint pain.
If there is severe inflammation, corticosteroids can also be prescribed that help in restoring the joint function. Supportive strategies, including jaw exercises and physical therapy can reduce stiffness of muscles and enhance joint mobility. Warm compressors and cold packs can also provide relief.
Oral appliances, such as dental splints or night guards can reduce grinding of teeth and prevent TMJ stress. Skeletal muscle relaxants can also reduce jaw tension.
Supportive measures include,
- Managing the stress levels
- Following an anti-inflammatory diet
- Intake of nutritional supplements

What are the complications of untreated TMJ pain in Lyme disease?
Several complications can occur when TMJ pain is left untreated. Severe inflammation can lead to joint stiffness and restriction in activities, such as chewing or talking. There can also be breakdown of cartilage and articular disc displacement.
If there is nerve involvement, facial pain or tingling sensation can occur. Patients also suffer from anxiety, disturbed sleep, and depression that contribute to poor quality of life.
When there is a failure in detecting Lyme disease at an early stage, the infection spreads and contributes to neuroborreliosis and systemic symptoms.
What imaging techniques are used in analyzing TMJ involvement in Lyme disease patients?
Magnetic Resonance Imaging is regarded as an effective imaging technique for evaluating TMJ involvement. MRI can provide brief information about the soft tissues and articular disc. It can also help in detecting the clinical signs of inflammatory arthritis.
Computed tomography can help in evaluating bony changes, such as sclerosis and narrowing of the joint space. In advanced cases, a CT scan reveals bony destruction or deformities.
Panoramic radiography helps in analyzing the associated structures that help in detecting the causes of orofacial pain. This technique can help in evaluating bony changes, condylar asymmetry, trauma, hypoplasia, etc.
Conclusion
Temporomandibular joint pain is a clinical manifestation of Lyme disease. When the condition is misdiagnosed, the treatment outcomes will be affected. Hence, it is important to understand the connection between Lyme disease and TMJ pain to initiate accurate interventions.
References
- Johns Hopkins Medicine. Temporomandibular disorder (TMD) [Internet]. Baltimore (MD): Johns Hopkins Medicine; [date unknown] [cited 2025 Jul 16]. Available from: Click here
- Cleveland Clinic. Temporomandibular disorders (TMD): overview [Internet]. Cleveland, OH: Cleveland Clinic; [date unknown] [cited 2025 Jul 16]. Available from: Click Here
- Roth HS, Hovenga R, Singer SR. Acute arthritis of the right temporomandibular joint due to Lyme disease: a case report [Internet]. Cureus. 2021 Jun [cited 2025 Jul 16];13(6):e?–?. Available from: Click Here
- Mayo Clinic Staff. TMJ disorders – diagnosis and treatment [Internet]. Rochester, MN: Mayo Clinic; Dec 24, 2024 [cited 2025 Jul 16]. Available from: Click Here
- Talmăceanu D, Lenghel LM, Bolog N, Hedeșiu M, Buduru S, Rotar H, Baciut M, Baciut G. Imaging modalities for temporomandibular joint disorders: an update. Clujul Med. 2018 Jul;91(3):280–7. doi: 10.15386/cjmed‑970. PMID: 30093805; PMCID: PMC6082607. Available Here


