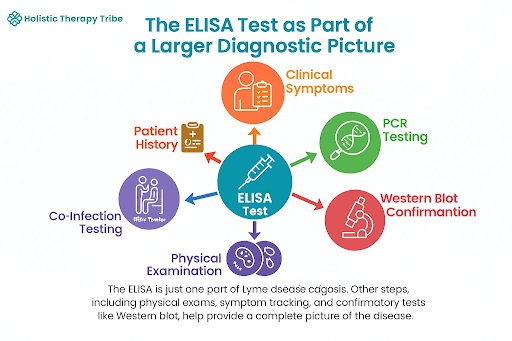
The& ELISA test is your first step toward understanding Lyme disease, but it’s just the beginning of the journey. With Lyme’s tricky symptoms, a clear diagnosis takes more than one test. From physical exams to confirmatory tests, each piece helps uncover the full picture. Let’s explore how the ELISA test fits into the larger diagnostic process and what it really tells you!
How the ELISA Test Works
Enzyme- Linked Immunosorbent Assay (ELISA) is the common method to identify the presence of antibodies in the blood. This will be a sign of the existence of an infection like Lyme disease. This operation is based on the use of the immune system of the body to detect certain proteins or pathogens. Blood Sample: A drop of blood is taken out of your vein and the most common site to get the blood sample is your arm. Laboratory Processing: The sample is sent into the laboratory and it is incubated with the antigens which are applicable to the bacteria that cause the Lyme disease, Borrelia burdorferi. Antibody Binding: Informatively, in the case that one is infected with Lyme disease, the body will start producing antibodies (IgM and IgG). This is because these antibodies react with the antigens hence giving positive results. Antibodies Detection: The plate is washed and secondary antibodies should be added. An enzyme -linked reaction is carried out thus resulting in change of color. This is because the antibodies present in the blood of the patient get attached to the antigen. Outcome: The Lyme disease is confirmed by the color change that denotes presence of Lyme disease. The level of color intensity is affected by the quantity of the antibodies used.

Factors That Can Affect Your Test Results Test time: In the early stages of Lyme disease, the body’s immune system might have not developed sufficient antibodies that the ELISA test was able to detect. Due to the possibility of false, adverse test outcomes, there is a likelihood of giving wrong, negative results despite the individual being infected. In case Lyme disease is suspected, then the test would require repetition or confirmation test. One of the instances is that in severe cases of Lyme disease the body generates an elevated quantity of antibodies that can be detected. It may also fail to give the right results in certain cases. It is rather essential to depend on clinical symptoms and test results. 2. False positives and Cross- Reactivity: Cross- Reactivity occurs when the immune system reacts to similar antigen in Borrelia burgdorferi bacteria to make the antibodies attach to it. This leads to false positive results during which the tests may give the developer of the tests a positive result suggesting that he or she has Lyme disease though he or she does not have it. 3. Diagnostic finding and laboratory result: ELISA forms a constituent of the diagnostic procedure. Clinical presentation like the classical signs and symptoms of Lyme disease are important aspects that should be taken into consideration. Physicians will not always take the lab report into complete consideration but they will also consider the history and symptomatic presentation of the patient in order to give a conclusive diagnosis.
What Happens After the Test?
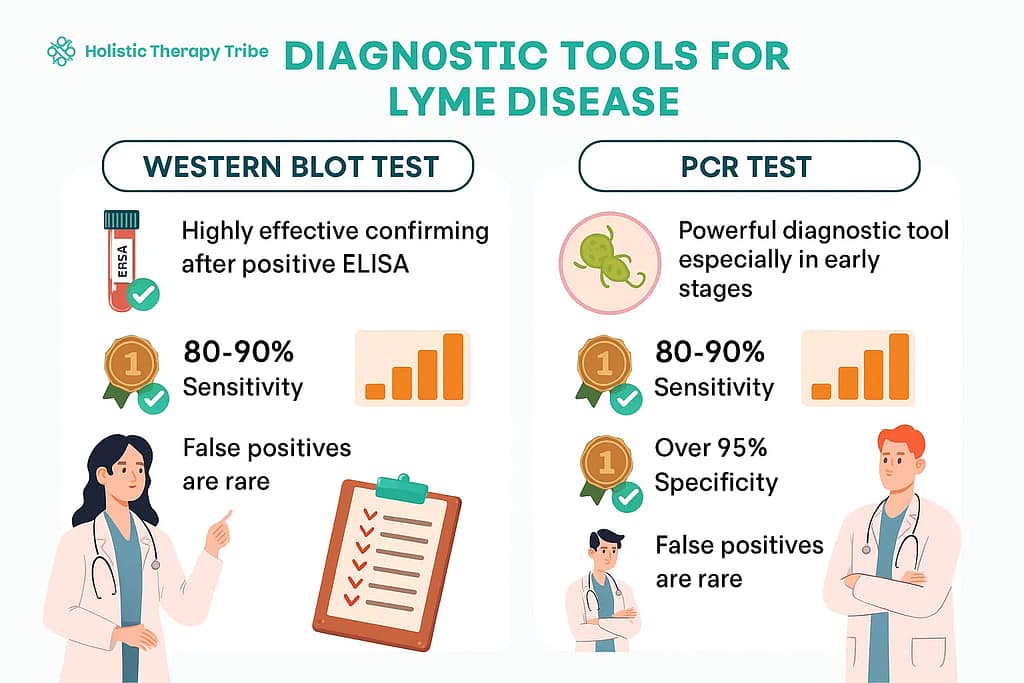
Confirmatory Testing: Western Blot Test- The ELISA test can therefore be positive or indeterminate, in such an event, a follow-up with western blot test is recommended. It is also more circumscribed and assists in validating the existence of the bacteria. It establishes whether the antibodies identified in the ELISA are associated with Lyme disease or whether it is cross-reactivity by the other infections. Polymerase Chain Reaction (PCR)- Where Lyme disease is suspected and the result is unknown during the early stages, a PCR test is applied. It is more receptive in recognizing Lyme disease during its start up phases when the indications are intense. 2. Next steps: Based on the mix of the symptoms and the laboratory findings, the medical history-a diagnosis is arrived at.Chronic Lyme may cause neurological and psychosocial symptoms that are brought about by untreated Lyme.
How long does it take to get a proper Lyme diagnosis?
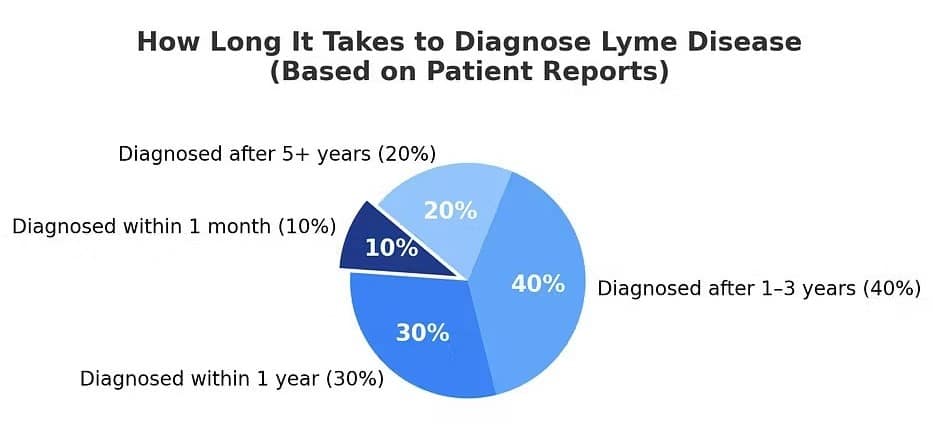
Its correct diagnosis of Lyme requires time because initially the afflictions do not appear permanent in nature. Subsequently, there may be possibilities that the laboratory tests and evaluation demonstrate false negative outcomes. In general it is a long process to actually make the correct diagnosis on a person with Lyme illness. Many patients would take an average of about 1 to 3 years before their lyme illness is diagnosed. This means that in case of suspicion of Lyme disease- find the symptoms, have specially designed tests or consult a doctor. The availability of the proper care can possibly work wonders in recovery.
Conclusion The importance of diagnosis of Lyme disease is accurate and in time. Each of the ELISA, Western Blot, and PCR have a critical role to play in reinstating the presence of Borrelia burgdorferi, the streptococcal bacteria which causes Lyme disease. Although the ELISA test is an effective screening test, the western Blot and PCR also provide accurate information, particularly on confirming the diagnosis, as well as knowing the active phases of the disease. In the end, we can say that although Lyme disease is controversial, the knowledge of the act on the tests and the significance of the early diagnosis can help a lot to prevent the development of long-term complications.
What’s Next for You?
Ready to explore a more complete path to recovery? Join the Lyme Support Network Community.
References
CDC. 2024. “Signs and Symptoms of Untreated Lyme Disease.” Lyme Disease. May 15, 2024. https://www.cdc.gov/lyme/signs-symptoms/index.html.
CDC. 2024. “Testing and Diagnosis for Lyme Disease.” Lyme Disease. May 20, 2024. https://www.cdc.gov/lyme/diagnosis-testing/index.html.
Alliance, Global Lyme. n.d. “Lyme Disease Diagnosis – Global Lyme Alliance.” Www.globallyme alliance.org. [GLA]
Center, Johns Hopkins Lyme Disease Research. 2020. “Think the Lyme Disease Rash Is Always a Bullseye? THINK AGAIN!” Johns Hopkins Lyme Disease Research Center. May 7, 2020. [Johns Hopkins Lyme Disease].
Rebman, Alison W., Ting Yang, Isaac Yoon, Debra Powell, Steven A. Geller, and John N. Aucott. 2023. “Initial Presentation and Time to Treatment in Early Lyme Disease.” The American Journal of Tropical Medicine and Hygiene 108 (4): 734–37. https://doi.org/10.4269/ajtmh.22-0437.


