If you are chronically feeling ill, inflamed, exhausted, or stuck in a cycle of recurring symptoms of Lyme disease– if you have been diagnosed with Lyme disease.
Lyme disease is a bacterial infection and Epstein- Barr is a viral infection causing mononucleosis.
In fact both the conditions do not just affect the body– they interrupt the immune system deeply.
In this guide, we will explore what is Epstein- Barr virus (EBV), the interlink between EBV and Lyme disease, the diagnosis, and how one can get support from various resources/ tools.
What Is Epstein-Barr Virus (EBV)?
- Epstein- Barr Virus, a common virus in the world– belongs to the herpesvirus family, best known as the cause of mononucleosis.
- The virus never fully goes away from your body, it stays in the dormant state in your cells. It can recur later in life when the immune system is low or weakened by other conditions and illness.
- While EBV is active in the body– either during the infection or a reactivation, it showcases a wide range of symptoms.
- Common Symptoms & Long-Term Impacts. Take a look:
| Typical Symptoms of Active EBV | Potential Long-Term Impacts |
|---|---|
| Severe fatigue that doesn't improve with rest | Chronic fatigue and post-viral symptoms |
| Swollen lymph nodes | Increased vulnerability to autoimmune conditions (e.g., lupus, Hashimoto’s) |
| Sore throat | Persistent cognitive issues ("brain fog") |
| Headaches or migraines | Anxiety |
| Low-grade fever | Mood shifts |
| Muscle aches and joint pain | Reactivation during times of stress, trauma, or other infections (like Lyme) |
| Rash | Liver or spleen inflammation |
Epstein-Barr (EBV) and Lyme disease: how are they connected?
Because these symptoms are non-specific and fluctuate over time, it’s common to be told it’s just stress, aging, or even psychosomatic. But for many, it’s the combination of EBV and Lyme—not just one or the other—that’s responsible for the long-term health spiral.
Epstein-Barr virus (EBV) and Lyme disease are connected through immune system disruption. Lyme disease, a bacterial infection from tick bites, can weaken immunity and trigger reactivation of latent EBV, leading to chronic symptoms like fatigue, joint pain, and cognitive issues. This overlap complicates diagnosis and treatment, especially in patients with persistent illness.
Immune Suppression & Viral Reactivation
- One of the overwhelming parts of chronic illness is the feeling that your symptoms are not just from just one thing– but rather from complex and varied issues.
- If there is Lyme disease and if it is followed by co- infections— this puts stress on the immune system. And this weakens your body which can ultimately give rise to dormant illness such as EBV. Thereby a second layer of illness is caused that might be just as disruptive as Lyme disease itself.
- This can also happen the other way around. If EBV reactivates prior- due to stress, trauma, or deprived immune function.
The Overlap: Why EBV and Lyme Often Show Up Together
Because these symptoms are non-specific and fluctuate over time, it’s common to be told it’s just stress, aging, or even psychosomatic. But for many, it’s the combination of EBV and Lyme—not just one or the other—that’s responsible for the long-term health spiral.
Immune Suppression & Viral Reactivation
- One of the overwhelming parts of chronic illness is the feeling that your symptoms are not just from just one thing– but rather from complex and varied issues.
- If there is Lyme disease and if it is followed by co- infections— this puts stress on the immune system. And this weakens your body which can ultimately give rise to dormant illness such as EBV. Thereby a second layer of illness is caused that might be just as disruptive as Lyme disease itself.
- This can also happen the other way around. If EBV reactivates prior- due to stress, trauma, or deprived immune function.
Shared Symptoms That Create Confusion
One reason EBV and Lyme are so often confused—or seen as one continuous illness—is that they share many of the same symptoms. This overlap can lead to misdiagnosis, under-treatment, or a focus on the wrong illness altogether.
Here are some of the most common symptoms shared by both EBV reactivation and chronic Lyme:
Support Tools and Resources
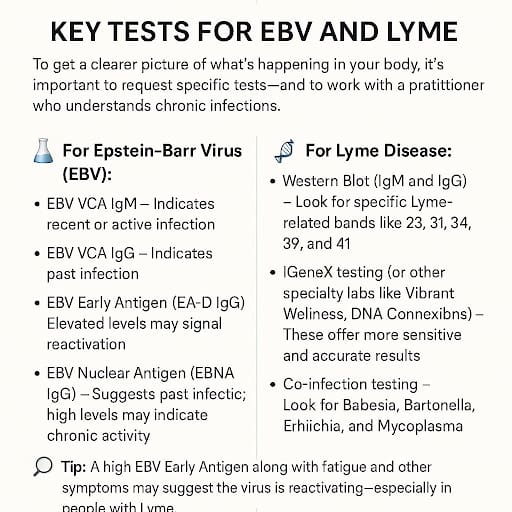
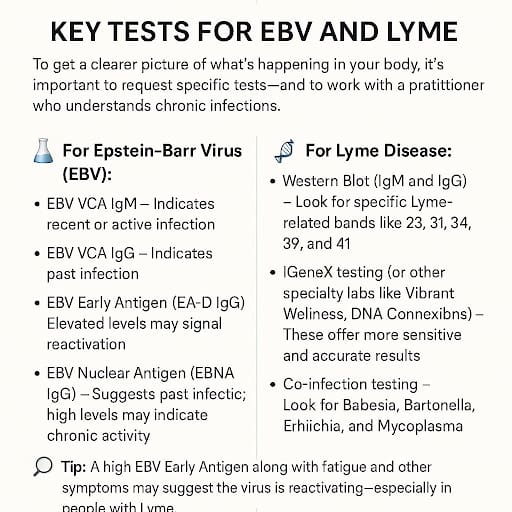
Diagnosing the Chronic Illness and EBV
If you are dealing with persistent symptoms like fatigue, brain fog, and pain, it is not uncommon to be passed from doctor to doctor without a clear answer. Unfortunately, both Epstein-Barr Virus (EBV) and Lyme disease are notorious for being underdiagnosed or misdiagnosed- especially when they occur together.
Here’s why:
- Symptoms are vague and overlap with many other conditions like fibromyalgia, chronic fatigue syndrome (ME/CFS), depression, or autoimmune disorders.
- Standard blood tests may come back “normal,” even when your body is struggling.
- Many doctors aren’t trained to recognize chronic or reactivated EBV, often dismissing it as a past infection that “shouldn’t cause problems.”
- Lyme tests can be unreliable, especially in chronic or late-stage infections, where the bacteria may suppress your immune response, causing false negatives. When both infections are at play, they can mask or amplify each other, making it incredibly difficult to pinpoint the root cause.
Key Tests for EBV and Lyme (And What to Ask For)
- Bitten by Kris Newby.
- Recovery from Lyme Disease: The Integrative Medicine Guide to Diagnosing and Treating Tick-Borne Illness by Daniel A. Kinderlehrer MD.
- Gone in a Heartbeat by Neil Spector, MD – memoir of a physician’s Lyme journey.
- Lyme Disease: An Evidence-based Approach, John J. Halperin (ed.)
- LymeDisease.org : Physician directory connecting patients to Lyme-literate doctors—free registration required.
- ILADS (International Lyme & Associated Diseases Society) : Global provider search for experienced Lyme specialists.
- Lyme Support Network Community Awareness, Prevention & care : Provides free registration, literature database, Lyme specialists and guidance.
- Global Lyme Alliance : Specialist locator for precision diagnosis and treatment.
- Lyme Disease Research Center (Johns Hopkins): Clinical studies and trials (referenced via cited books).
- Lyme Support Network Community (Holistic Therapy Tribe) : Virtual meetings, Facebook, Twitter, group networks.
- Patient.info (Lyme Discussions) : One example of patient-experience threads (“feel like I’m dying”)
- LymeForums.org : Active category-based forums with threads on diagnosis, living with Lyme, etc.
Sample Symptom Tracker
Tracking your symptoms can help identify patterns, evaluate treatment progress, and improve communication with your provider. Use a journal, spreadsheet, or app like Lyme Symptom Tracker.
Daily Symptom Log Template
| Sr. No. | Date | Fatigue (scale 1–10) | Brain Fog | Joint Pain | Sleep (hours) | Mood | Supplements Taken | Notable Triggers | Overlapping Symptoms with other Illness |
|---|---|---|---|---|---|---|---|---|---|
| 1 | |||||||||
| 2 |
- Menstrual cycle phase (for hormonal influence)
- Weather/barometric pressure
- Food sensitivities
- Detox reactions (herxheimer symptoms)
Conclusion
- Misdiagnosis does not mean that there is no hope.
- Your symptoms are real. Your story matters. And even if the road towards proper and final diagnosis is long– it is never too late.Keep asking questions. Keeping seeking answers.
What’s Next for You?
Ready to explore a more complete path to recovery?
References
- CDC. 2024. “Signs and Symptoms of Untreated Lyme Disease.” Lyme Disease. May 15, 2024. Link.
- CDC. 2024. “Testing and Diagnosis for Lyme Disease.” Lyme Disease. May 20, 2024. Link.
- Alliance, Global Lyme. n.d. “Lyme Disease Diagnosis – Global Lyme Alliance. [GLA]
- Center, Johns Hopkins Lyme Disease Research. 2020. “Think the Lyme Disease Rash Is Always a Bullseye? THINK AGAIN!” Johns Hopkins Lyme Disease Research Center. May 7, 2020. [Johns Hopkins Lyme Disease].
- Rebman, Alison W., Ting Yang, Isaac Yoon, Debra Powell, Steven A. Geller, and John N. Aucott. 2023. “Initial Presentation and Time to Treatment in Early Lyme Disease.” The American Journal of Tropical Medicine and Hygiene 108 (4): 734–37


