
When an unusual rash appear on the skin, it is normal to feel confused by thinking about the condition. According to the Center for Disease Control and Prevention, around 30,000 new cases are reported every year. Even though Lyme disease is not an autoimmune disorder, the clinical symptoms of Lyme disease may mimic an autoimmune condition.
Presence of skin rashes also indicate psoriasis, which is an autoimmune disease. Can Lyme disease trigger psoriasis? There is a high chance of misdiagnosis due to the similarity in the clinical symptoms. In this blog, we will explore together how Lyme disease and psoriasis are related.
What is psoriasis?
Psoriasis is an autoimmune condition which is characterized by inflamed regions. When the skin cells proliferate quickly, it will shed every 3 to 4 days. (1) The clinical symptoms involves:
- Itching
- Dry skin
- Pitted nails
As psoriasis is an autoimmune condition, the immune system attacks healthy cells, resulting in inflammation or swelling. Triggering factors for psoriasis can include:
- Stress
- Presence of an underlying infection
- Skin injury
- Certain medicines

Can a tick bite trigger autoimmune condition?
Post-treatment Lyme disease syndrome is believed to be immune-mediated. Some patients may develop rheumatoid arthritis, neuropathy etc. When the immune system of the host is exposed to spirochetes for a long time, it can lead to chronic autoimmune conditions.
Case study:
A 35-year old woman consulted a specialist with the complaints of skin rashes, weakness, fever, etc. The doctor prescribed steroids for one month, but the clinical symptoms didn’t improve. The blood tests revealed increased WBC count, and ESR (erythrocyte sedimentation rate).
The patient was diagnosed with Lyme disease followed by a course of antibiotic therapy. After two months of antibiotic treatment, the patient presented with erythema, fever, pain, etc. The patient underwent a skin biopsy.
Through direct immunofluorescent study, immunoglobulins were found in the basement membrane. The clinical symptoms and diagnostic data revealed an autoimmune condition, called systemic lupus erythematosus (SLE). The doctor recommended a combination of vitamin D, calcium, and prednisolone.
Why do people with Lyme disease develop psoriasiform lesions?
According to the studies, people with Lyme disease develop psoriatic arthritis. The rashes can result in skin discoloration. In the later stages of Lyme disease, sclerotic lesions are observed that mimic psoriasiform lesions.
Case study:
A 70-year old man was given a diagnosis of psoriatic arthritis and was prescribed corticosteroids and methotrexate. But, the clinical symptoms didn’t improve. The introduction of tumour necrosis factor alpha inhibitor treatment made the clinical symptoms worse.
At this stage, skin biopsy was performed that confirmed the diagnosis of Lyme disease. Ten days of antibiotic treatment was intitiated that led to better prognosis. (4)
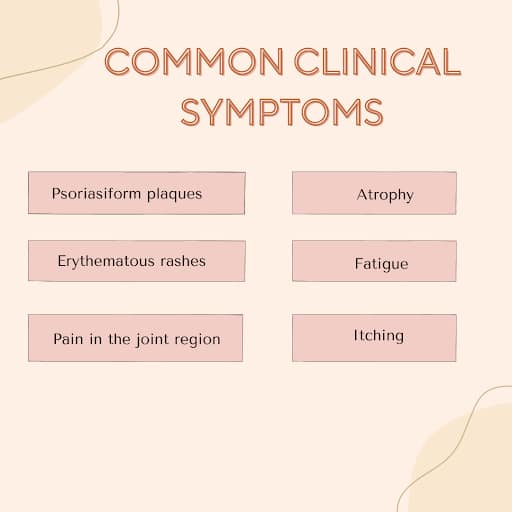
What are the clinical symptoms of Lyme disease that mimic psoriasis?
Several symptoms of Lyme disease may mimic psoriasis that makes diagnosis challenging.
- Psoriasiform plaques
- Erythematous rashes
- Pain in the joint region
- Atrophy
- Fatigue
- Itching
How is the management of Lyme disease different from psoriasis?
The management of Lyme disease varies from psoriasis due to the difference in underlying causes. Psoriasis is an autoimmune condition whereas Lyme disease is caused due to a bacterial infection. The treatment for psoriasis include corticosteroids, methotrexate, managing stress levels, vitamin D supplements, etc.
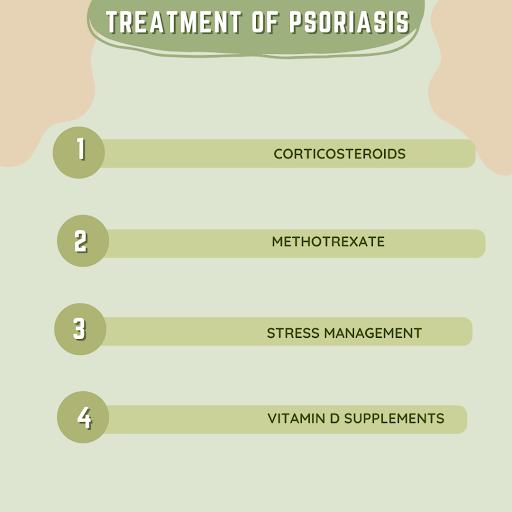
When the lesions are widespread, or resistant, phototherapy can be used. The treatment of Lyme disease includes antibiotics.
Antibiotics can be prescribed orally or intravenously for relieving the clinical symptoms. The treatment of psoriasis involves the suppression of the immune system to control inflammation.
Management of lyme disease depend on the strength of immune system and antibiotics to eliminate infection.
What happens when Lyme disease and psoriasis occur simultaneously?
When Lyme disease and psoriasis co-exist, they present a twisted relationship between infection-induced inflammation and auto immunological dysregulation that makes diagnosis and treatment difficult. These diseases affect the immune system, although in different directions. Lyme disease can activate psoriatic flares, in part via immune processes where bacterial proteins appear similar to human skin proteins, which causes dilemma to the immune system.
The treatment of psoriasis is often achieved through the use of **immunosuppressive drugs** or **biologics** (e.g. TNF- 1 alpha inhibitors or IL- 17 inhibitors). Nevertheless, these treatment options can damage the immune system to combat Borrelia and cause delayed healing or lifelong illness. Conversely, antimicrobial agents cannot affect autoimmune pathways of psoriasis.
Besides, the patients with the two conditions are at risk of developing psoriatic arthritis and Lyme arthritis, which are the conditions characterized by swollen and stiff joints. Finally, the treatment requires a multidisciplinary approach that involves dermatologists, rheumatologists, etc.
Conclusion:
Due to the similarity in the clinical symptoms, it is difficult to diagnose and manage Lyme disease and psoriasis. There is a vast difference in the origin of both the conditions. Lyme disease is caused by bacterial infection, whereas psoriasis is an autoimmune condition. When your skin is showing signs of inflammation, seek medical help that can lead to better prognosis and improved quality of life.
References:
- Johns Hopkins Medicine. Psoriasis. Baltimore (MD): Johns Hopkins Medicine; [date unknown; cited 2025 Jun 17]. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/psoriasis
- Cleveland Clinic. Psoriasis. Cleveland (OH): Cleveland Clinic; [date unknown; cited 2025 Jun 17]. Available from: https://my.clevelandclinic.org/health/diseases/6866-psoriasis
- Lantos PM, Lipsett SC, Fancher TL, Schechter MA, Hsieh DT, Smith JD, et al. Lyme borreliosis as a trigger for autoimmune disease. Eur J Intern Med. 2022;101:10–17. [Cited 2025 Jun 17]. Available from: https://pubmed.ncbi.nlm.nih.gov/PMC8578812/
- Steppat A, Skaarup Andersen N, Andreasen CM. Rare case of Lyme borreliosis in a patient presenting with dactylitis and skin rash. BMJ Case Rep. 2023 Feb 17;16(2):e253182. [cited 2025 Jun 17]. Available from: https://casereports.bmj.com/content/16/2/e253182


