Lyme disease is often characterized by clinical symptoms, such as skin rashes and flu-like symptoms. Sometimes, the bacteria can reach the nervous system and cause neurological complications. The bacterial infection can cause spinal degeneration, which is characterized by tingling sensations, and back pain.
What happens when this condition is left untreated? Is it possible to diagnose this condition at an earlier stage? In this blog, we will explore how Lyme disease can result in spinal degeneration.
Can Lyme disease cause spinal degeneration?
Lyme disease is spread to humans through a tick bite that can cause chronic complications if left untreated. The clinical symptoms include
- Erythema migrans (skin rashes)
- Musculoskeletal pain
- Brain fogFever
- Paralysis of the facial nerve (Bell’s palsy)
- Numbness
When left untreated, Lyme disease can cause degeneration of the spine. When the infection progresses, there will be oxidative stress. This results in the disruption of spinal cells. As a result, the disc will lose its elasticity.
When the bacteria cross the blood-brain barrier, it can result in neuroborreliosis. The nerve roots and spinal cord can become inflamed. When the inflammation is chronic, the protective layers of nerves and spinal cord will be damaged.
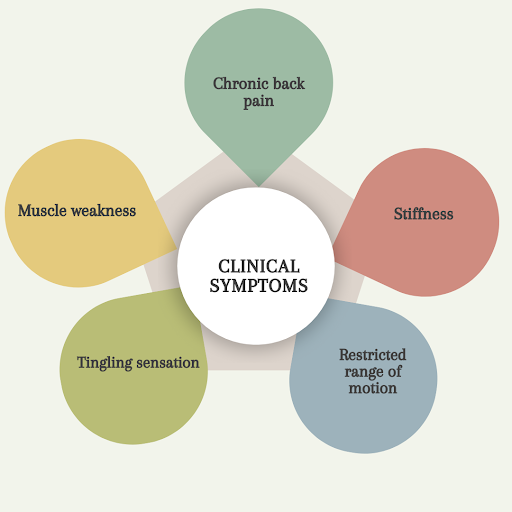
Clinical symptoms of spinal degeneration:
Depending on the severity, spinal degeneration can result in several clinical symptoms:
- Chronic back pain: The pain may be localized to one particular region, or it can also radiate to distinct parts.
- Stiffness
- Restricted range of motion: Individuals with spinal degeneration find it difficult to move.
- A tingling sensation can be experienced in the upper or lower extremities
- Spinal degeneration can also make the muscles weak which makes it difficult to perform daily activities.
How is spinal degeneration in Lyme disease diagnosed?
Normally, spinal degeneration can be diagnosed with the help of MRI or a CT scan. These tests can help the doctors to evaluate the alignment of the discs. If Lyme disease is suspected, a spinal tap or lumbar puncture can be performed to confirm the infection.
Spinal tap for Lyme disease:
Spinal tap is a diagnostic test that uses a sample of cerebrospinal fluid to detect the presence of antibodies. CSF is a clear fluid that flows around the brain/spinal cord. A CSF test can be conducted to analyse whether the infection has reached the nervous system.
Procedure:
- The patient can lie or sit on a table.
- After cleaning the back area, an anesthetic will be injected into the skin. A numbing cream can also be applied before the injection.
- When the area is numb, a hollow needle will be inserted between the 2 vertebrae in the lower spine
- A minimal amount of CSF will be obtained for the test, which approximately takes 5 minutes.
- After the procedure, it is important to rest for 1 or 2 hours.
There can be a slight tenderness at the site of injection. Sometimes, there is a chance of a headache that can last for hours or weeks.
| Positive result | The antibodies against the bacteria were detected in the CSF. If there are more antibodies in the CSF than blood, the infection has reached the nervous system. |
| Negative result | Antibodies were not detected in the CSF. |
Is a spinal tap for Lyme disease useful in early or late stages of infection?
Usually, a spinal tap is not conducted in the early stages of infection. Erythema migrans or bull’s eye rashes can suggest infection. At this stage, oral antibiotics can be administered. When the infection progresses, neurological symptoms appear. Antibodies require a certain period to form in the body against the bacteria. Hence, a CSF test may not be reliable in the early stages.
Later stages of infection can be characterized by cognitive dysfunction, radicular pain, etc. Antibodies (IgG and IgM) can be easily detected in the later stages of infection. Spinal tap is not commonly used to detect early stages but rather can be termed as an excellent diagnostic tool in later stages.

What are the treatment options for spinal degeneration in Lyme disease?
If the diagnosis of Lyme disease is confirmed, antibiotic therapy must be initiated. These medicines can be administered orally or intravenously. This can help in preventing further disease progression.
A physiotherapist can recommend muscle strengthening programs that support the spine. Medications such as non-steroidal anti-inflammatory drugs and steroids can help relieve the symptoms. When steroids are injected near the spinal nerves, pain/inflammation will be reduced.
Acupuncture involves inserting the needles at specific points in the body that help improve blood circulation. Techniques like spinal adjustments can enhance mobility. Gentle stretching and yoga can help in correcting the posture.
‘If nonsurgical treatment options have failed, surgical options can be considered.
| Diskectomy | Removal of the portion of the spinal disk that helps in relieving pressure |
| Laminectomy | Removal of minimal amount of bone from the lower spine |
| Spinal fusion | Connecting the vertebrae that helps in providing stability |
| Foraminotomy | The bone and tissue near the opening of the nerve roots will be removed. |

What are the complications of spinal degeneration in Lyme disease?
Chronic back pain is one of the musculoskeletal complications of untreated spinal degeneration. It can cause a reduction in disc height, leading to instability in the spine. With the progression of the disease, patients undergo limited mobility and stiffness of the lumbar spine. Myelopathy might even develop in severe cases of the disease, which results in spinal cord failure.
The spinal degeneration in Lyme disease can mimic autoimmune disorders. Hence, there is a high risk of misdiagnosis. Mental health problems, like depression or anxiety can occur due to persistent pain. Timely diagnosis is important to initiate the treatment at an early stage.
Diagnostic techniques, like lumbar puncture can help in diagnosing spinal degeneration. After confirming the diagnosis of Lyme disease, antibiotic therapy can be recommended at an early stage.
Conclusion:
- Lyme-disease causing bacteria can reach the central nervous system and lead to spinal degeneration.
- Spinal tap for Lyme disease has become an essential tool to analyse the involvement of nervous system in the later stages.
- If the infection is identified at an early stage, an appropriate treatment plan can be indicated to prevent complications.
References:
- Contreras F. Lyme Disease Spinal Degeneration: Causes & Solutions. Oasis Medical Institute [Internet]. ca. 1.6 years ago [cited 2025 Jul 30]. Available from: https://oasismedicalinstitute.com/lyme-disease-spinal-degeneration/
- Cleveland Clinic. Degenerative Disk Disease: What It Is, Symptoms & Treatment [Internet]. Published ca 5 months ago [cited 2025 Jul 30]. Available from: https://my.clevelandclinic.org/health/diseases/16912-degenerative-disk-disease
- MedlinePlus. Lyme Disease Tests [Internet]. Reviewed 2023 Jun 1 [cited 2025 Jul 30]. Available from: https://medlineplus.gov/lab-tests/lyme-disease-tests/