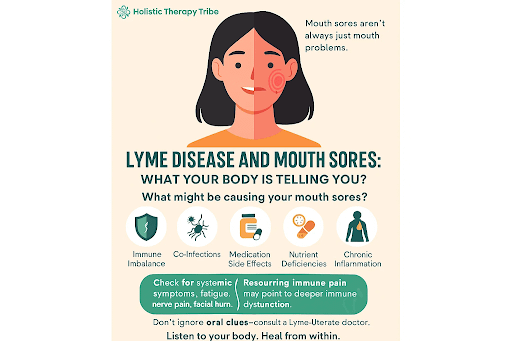
Mouth sores seem to be a small nuisance. Isn’t it? But for someone living with Lyme disease, they could be a sign of something deeper.
Right from burning sensations to recurring ulcers and so on– your mouth can be a mirror that can actually reflect what your body holds within.
Figuring out what might as well cause it, what might actually help!
We will explore which remedies can bring relief, what is their relation, how detox and healing can play an important role in your recovery.
The Science Behind Oral Symptoms and Lyme

- Borrelia burgdorferi bacteria can affect the cranial nerves (mainly the facial nerve), and sometimes TMJ.
- In some Lyme patients, burning mouth syndrome is related to neurological involvement due to Lyme bacteria. However, there is no causal pathway that has been proven for this interlinkage. Orofacial features are quite uncommon and non- specific in nature.
- How Lyme affects Immune system and Oral Inflammation
- The bacteria affects the immune system by interfering with immune signaling.
- That triggers chronic inflammation and elevates the cytokines that affect the tissues throughout the body (including oral mucosa).
- Mouth sores are rare. But systemic inflammation and imbalances in the immune system can cause conditions such as oral irritation, burning mouth syndrome, or slow- healing lesions in few individuals.
4. Role of Co-Infections & Immune Suppression
- Common co-infections like Babesia, Bartonella, and Mycoplasma lead to distortion in the immune system that can worsen the symptoms and prolong the recovery period.
- The tick suppresses local immunity and can lead to opportunistic infectious conditions in areas such as the mouth, and so on.
- This weakens the oral barrier, thereby increasing vulnerability to sores, oral thrush, and so on. Although, the direct links are under investigation and there is scope of research.
Common vs. Uncommon Orofacial Manifestations

| Orofacial Symptom | Frequency in Research (Lyme) | Notes |
| Facial palsy | ~42 % | One of the most frequent neurologic signs in Lyme patients |
| TMJ pain / temporomandibular disorder | ~42 % | May mimic typical TMD; can lead to misdiagnosis |
| Headache | ~39.5 % | Common systemic as well as local symptom |
| Altered taste (dysgeusia) | ~11 % | Reported in a subset of patients |
| Sore throat / neck pain | ~3 % / ~7.5 % | Nonspecific oropharyngeal complaints |
| Burning mouth syndrome | Rare (few case reports) | Hypothesized neural involvement but not proven |
| Mouth ulcers / aphthae | Extremely rare | Only isolated case reports exist (e.g. pediatric case) |
When Mouth Sores Signal Something More Serious
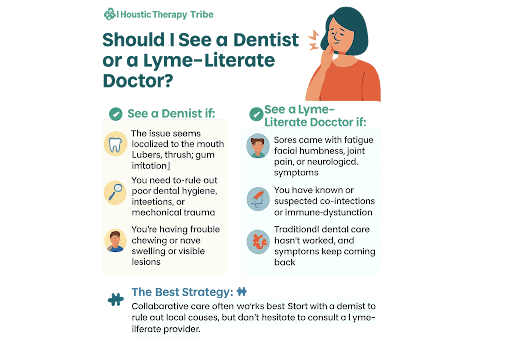
- Signs that might require Immediate Medical Attention
- Persistent mouth sores that are painful in nature last longer than 2 weeks.
- Sores bleed easily that are larger or recurring in nature.
- It is often accompanied by facial paralysis, numbness, or vision changes.
- If any of the oral conditions are not responsive to the treatment, that may indicate a condition of immune suppression in the body.
- Now, this might as well suggest something beyond typical inflammation which is usual in Lyme disease patients with co- infections or immune suppression cases.
2. Neurological Implications or Autoimmune responses
- Chronic Lyme triggers autoimmune responses potentially causing mouth ulcers similar to lupus, Behçet’s disease, or lichen planus.
- Neurological Lyme or Neuroborreliosis
- Co-infections like Epstein-Barr Virus or Bartonella can contribute to systemic immune dysfunction, increasing risk for autoimmune-like oral conditions.
Treating Mouth Sores in Lyme: What Works and What Doesn’t
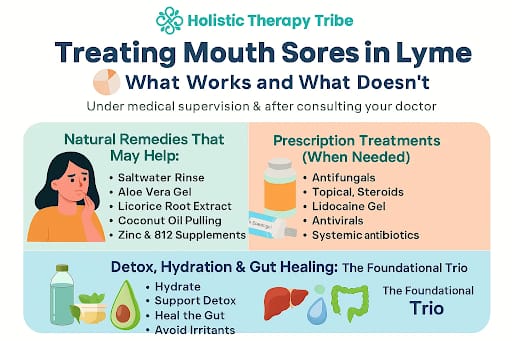
- Natural Remedies That May Help: Natural remedies are quite useful in the cases where the sores are minor and yet recurrent in nature. Natural remedies are gentle and low- risk options.
- Saltwater gargles- reduces inflammation and promotes healing
- Licorice root extract- reduces pain and support healing, anti- inflammatory properties
- Aloe vera ge (oral- safe)- soothes the irritation
- Zinc lozenges and B12 supplements- aid if deficiencies are contributing to ulcers
- Coconut oil pulling- helps in enhancing oral microbiome and fights with candida infections effectively.
2. Pharmacological Treatment (when it is needed):
- Antifungals – if oral thrush or candida is diagnosed
- Topical corticosteroids – for painful, inflamed ulcers or autoimmune-like lesions
- Lidocaine gel/mouthwashes – temporary pain relief for severe soreness
- Antivirals – if sores are linked to HSV or EBV reactivation
- Systemic antibiotics – only if a secondary bacterial infection is present
3. Detox, Hydration & Gut Healing: The Foundational Trio
- Hydration- dry mouth deteriorates the irritation and delays the healing process
- Detoxification- supporting liver and lymphatic pathway detoxification through lemon water, herbal teas, dry brushing, and so on.
- Healing the gut- probiotics, bone broth, and an anti-inflammatory diet reduce oral and systemic inflammation
- Avoid irritants- acidic foods, alcohol-based mouthwash, and spicy foods can aggravate ulcers
Conclusion
- Treating mouth sores in Lyme isn’t just about soothing the surface—it’s about listening to your body’s signals and addressing the internal imbalances fueling them.
- Whether it’s a simple salt rinse or a deeper dive into detox and gut repair, the path to healing is as much about tuning in as it is about treating symptoms.
- Remember: when your mouth talks, your immune system might be whispering the truth behind the pain.
What’s Next for You?
Ready to explore a more complete path to recovery? Join the Lyme Support Network Community.
References
- Hijazi K, Patel J, Lal S. Orofacial manifestations of Lyme disease: Review for dental professionals. Dimensions of Dental Hygiene. 2021. Available from: Link
- Ashurst J, Perry M. Bilateral facial diplegia: A rare presenting symptom of Lyme. Case Reports in Infectious Diseases. 2017;2017:4521526. doi:10.1155/2017/4521526. Available from:Link
- Tracy KE, Baumgarth N. Borrelia burgdorferi manipulates innate and adaptive immunity to establish persistence in rodent reservoir hosts. Frontiers in Immunology. 2017;8:116. doi:10.3389/fimmu.2017.00116. Available from:Link
- Petnicki‑Ocwieja T, Kern A, Tryniszewska B, Behera AK, Koper KE, Cullen M, et al. The role of Toll‑like receptor 1 in early immune response to Borrelia burgdorferi infection. J Immunol. 2013;190(7):3373–3383. doi:10.4049/jimmunol.1202640. Available from:Link PubMed
- Raza M, Abbas M, Siddiqui AA, et al. Tick‑borne diseases and co‑infections: A growing threat. Pathogens. 2021;10(3):281. doi:10.3390/pathogens10030281. Available from:Link
- CDC. Clinical care and treatment of neurologic Lyme disease. Centers for Disease Control and Prevention (CDC). 2025. Available from:Link


